Building a Better BMI
 hood.isbscience.org/2023/03/20/biological-bmi/
hood.isbscience.org/2023/03/20/biological-bmi/ISB researchers have constructed biological body mass index (BMI) measures that offer a more accurate representation of metabolic health and are more varied, informative and actionable than the traditional, long-used BMI equation. The work was published in the journal Nature Medicine.
For decades, clinicians have relied on BMI as a crude tool to classify individuals as underweight, normal weight, overweight or obese. BMI scores are calculated by dividing a person’s weight in kilograms by height in meters squared. About 30 percent of the population is misclassified by this approach. Despite its limitations, BMI continues to be insightful and widely accepted in the clinic, as it is a major risk factor for a number of chronic diseases, including diabetes, cardiovascular diseases and cancer.
“For years, BMI has been the go-to measure for doctors to classify individuals based on their height and weight in comparison to an average person. However, this average person doesn’t truly exist. We now have the capability to use advanced molecular measurements as a more comprehensive representation of a person’s metabolic health, which can be used to make more accurate clinical recommendations for individuals,” said Noa Rappaport, PhD, ISB senior research scientist and corresponding author of the paper.
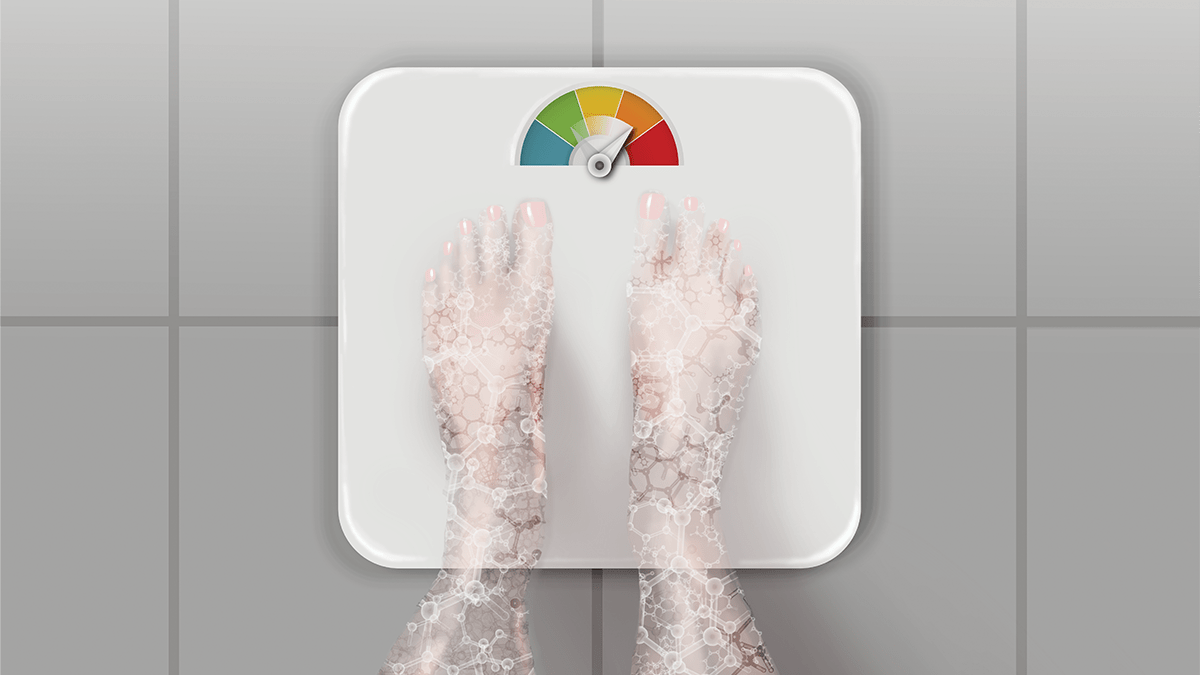
This illustration depicts a view we are all familiar with – looking down at one’s feet on a scale. However, the indicator of the body weight is replaced with a molecular layer indicating metabolic health status. The molecular layer, in this instance, is shifting to a worse value compared to the classical BMI – a reading that would otherwise be invisible without leveraging the underlying molecular data. (Art by Allison Kudla / ISB)
Rappaport and colleagues studied 1,000 individuals who enrolled in a wellness program by performing multi-omic profiling, examining more than 1,100 blood analytes such as proteins and metabolites, as well as genetic risk scores and gut microbiome composition collected at various time points. The researchers then generated machine learning models that led to more accurate predictive variations of a biological BMI than traditional measures of BMI alone.
The team made several important findings, including:
- Those with a high biological BMI and normal traditional BMI were less healthy, but able to lose weight easier following a lifestyle intervention.
- Those classified as obese with traditional BMI but with a normal biological BMI were more biologically healthy, and found it harder to lose weight.
- When people made positive lifestyle changes, biological BMI was more responsive and dropped earlier than traditional BMI.
With positive lifestyle changes, the findings suggest that even if someone is not losing weight, they may be getting healthier biologically.
“This work is a valuable asset for comprehending the molecular changes associated with obesity and metabolic health, and it has the potential to significantly improve the development of predictive and preventive clinical approaches for treating metabolic disturbances,” said Kengo Watanabe, PhD, lead author of the study and K. Carole Ellison Fellow in Bioinformatics.
Added Rappaport: “We have demonstrated the value of multi-omic profiling to reveal important insights into the complex relationships between obesity, metabolic health and chronic disease, and emphasized the need to consider a range of factors beyond traditional measures of BMI in understanding and addressing these issues.”